An aching soreness in your butt, shooting pain down the back of your leg. Irritation with every step when you run, sound familiar? These are the classic symptoms of piriformis syndrome. A stubborn and troublesome injury.
That can cause sciatica like pain. Pain that can radiate from your butt around your hip or all the way down your hamstrings and even into your lower leg.
Piriformis syndrome is tricky to diagnose, so statistics on its frequency are hard to come by. At best, it appears to account for no more than one to three percent of all running injuries.
One study of over 2,000 injured runners seems to have included it in the larger category of “sacroiliac injuries.”
Accounting for about one percent of injuries. Some cases may have also been misdiagnosed as gluteus medius pain, which accounted for just over three percent of injuries in the study.1
In any case, rare as it may be, piriformis syndrome is a real pain when you have it. So, what can you do about it?
Anatomy of Piriformis Syndrome
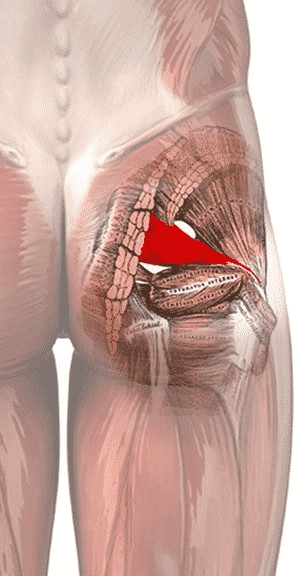
The piriformis is a small, narrow muscle that runs from just above your tailbone to the head of your femur. It helps externally rotate and abduct your hip. But it’s not the only muscle that does so. The gluteus medius and gluteus minimus are bigger, more powerful muscles that perform essentially the same function.
The piriformis (as well as these lesser glute muscles) also serve to stabilize your hip when you firmly plant your foot on the ground. Like during the stance phase of running.
If the piriformis is a weak, small, and seemingly unimportant muscle, how could it cause so much trouble? The piriformis does have one unique anatomical feature. Its proximity to the sciatic nerve. The sciatic nerve is the longest nerve in the body. Running from the base of your spine all the way down to your foot. Fore more, please read, Overcoming Sciatica.
As you might guess from its name, the sciatic nerve is also the source of the pain pattern we call sciatica. Aching or burning pain that radiates down the length of the sciatic nerve.2
The sciatic nerve passes right next to the piriformis. In fact, in somewhere between seven and 21% of the population, the sciatic nerve actually passes through the piriformis muscle.4
As a result, any aggravation or irritation of the piriformis muscle is likely to aggravate the sciatic nerve as well. Potentially causing localized pain in the piriformis region and sciatica pain down the back of the leg.
Piriformis Syndrome And Sciatica
It’s important to differentiate sciatica and piriformis syndrome in runners. Sciatica is a pain pattern. More of a symptom than an injury. Several things can cause sciatic nerve pain. The more common is a herniated disc in the lower back.
But piriformis syndrome is another one. Pain along the sciatic nerve is not the only symptom of piriformis syndrome. Nor should a lack of sciatic nerve pain be a reason to rule out piriformis syndrome.
According to a 2003 review study in the scientific journal Clinical Orthopaedics and Related Research, some of the key symptoms of piriformis syndrome include hip pain between the tailbone and the head of the femur, pain with hip flexion or internal rotation, and tenderness over the piriformis itself.
The pain will often get worse with sitting or squatting.3
One specific test for piriformis syndrome is the FAIR test. Which stands for flexion, adduction, and internal rotation. 4
Stretching the piriformis directly, as shown below, can also reproduce symptoms.4

When you run, the piriformis’ role as a hip stabilizer means that piriformis syndrome will cause pain during the stance phase of running. Because increasing stability is needed at higher speeds, the pain will likely get worse as you go faster.
Treating Piriformis Syndrome In Runners
Perhaps due to its rarity in athletes and its commonality among the general population, there are plenty of studies on treatment approaches for sedentary people. But relatively few among athletes. Among the general population, symptomatic relief is the primary focus.
Typical treatments involve physical therapy modalities like ultrasound, stretching, and injections of numbing, anti-inflammatory, or muscle relaxant medications.
One study, published in 2010 by Jason Tonley and other researchers at several clinics and universities in Los Angeles, describes a different approach for athletes.5
Tonely et al. note that though hip muscle weakness has been noted in numerous studies on people with piriformis syndrome, hip strengthening exercises are almost never included in standard physical therapy routines for the injury. Further, Tonley et al. propose that the piriformis becomes aggravated when it is overworked as a result of weakness in the other muscles that abduct and externally rotate the hip.
Improving Hip Muscle Strength
To bolster their argument, the authors cite research showing that hip muscle weakness is associated with a number of other hip and knee injuries. And even cite another study which found that including hip strength exercises in a rehab program for piriformis syndrome seemed to speed recovery.
To demonstrate how such a program might be put into practice, Tonley et al. outline how they used a hip strengthening program to treat a recreational athlete with the typical symptoms of piriformis syndrome.
Though it’s only a case study, Tonley et al.’s rehab program is still a good place to start for treating piriformis syndrome in runners. Their biomechanical argument is sound and the link between running injuries and hip muscle weakness has merit.
Tonley et al.’s rehab program can be augmented by other treatments advocated in other scientific papers, like massage, stretching, and injection of medications.
Please read The Relationship Between Hip Strength And Running Injuries for more.
RunnersConnect Insider Bonus
Download our Top 5 exercises to prevent piriformis injuries inside your Insider Members area.
It’s a PDF with images and descriptions of the 5 most effective prevention and rehab exercises for runners with Piriformis issues.
Aggressive Treatments For Piriformis Syndrome
If your piriformis syndrome does not abate after the stretching and strengthening program (per above), there are some second-line treatments you can try. Several scientific papers describe injecting lidocaine and corticosteroids directly into the piriformis to decrease pain and inflammation.3,4
This may be particularly helpful if you have sciatica type pain. Since inflammation of the piriformis is a known cause of sciatic nerve irritation. Though it’s important to note that these treatments were generally on sedentary people, not athletes.
Soft tissue manipulation techniques like massage, Active Release Technique, and Graston Therapy have been used by some runners to loosen up a tight piriformis muscle. Some runners even roll on a lacrosse ball or a baseball as a home remedy to get the same effect.
Though there’s been no formal research on the efficacy of any of these soft tissue techniques. Pushing too hard on the piriformis could cause further irritation of the sciatic nerve, so consider this before getting overzealous with soft tissue therapy.
In rare cases, surgery is helpful when piriformis pain is long-standing and does not respond to any other interventions. This is something you’ll have to discuss with a trusted doctor who has experience working with athletes.
Cross Training While Injured and During Recovery
Cross training is recommended while you're injured and as you slowly return to running.
The best form of cross training for this injury is Aqua Jogging. Studies have shown that aqua jogging can enable a well-trained runner to maintain running fitness for up to 4-6 weeks.
Aqua jogging is a form of deep water running that closely mimics the actual running movement. Your feet don’t actually touch the bottom of the pool, so it is zero impact and safe for almost any type of injury. In my experience, the only time to avoid aqua jogging is when you have a hip flexor injury, which can be aggravated by the increased resistance of the water as you bring your leg up. Because aqua jogging closely mimics natural running form, it provides a neuromuscular workout that, in addition to aerobic benefits, helps keep the running specific muscles active. The same can’t be said for biking and swimming. The only downside to aqua jogging is that you need a pool that is deep enough to run in without touching the bottom. If you’re lucky enough to have access to a pool of this size, aqua jogging should be your first cross training choice.In one study, a group of ten runners trained exclusively with deep water running for four weeks and compared 5km race times pre deep water running and post deep water running.
The researchers found no statistical difference in 5k time or other markers for performance, such as submaximal oxygen consumption or lactate threshold.
In a second study, researchers measured the effects of aqua jogging over a six week period.
This time, 16 runners were separated into two groups – one who did aqua jogging workouts and the other who did over land running.
Using the same training intensities and durations, the researchers found no difference between the groups in maximal blood glucose, blood lactate, and body composition.
It get’s better:
Research has also demonstrated that aqua jogging can be used as a recovery tool to facilitate the repair of damaged muscles after hard workouts.
These findings make aqua jogging an important recovery tool in addition to being the best cross training method for injuries.
Need one more reason?
The calories burned aqua jogging are even higher than running on land, so if you want to avoid weight gain while you take time off from running, this is definitely the exercise for you!
Aqua Jogging Workouts For Runners
If you're interested in aqua jogging to rehab your injury, then the absolute best way is to use one of my favorite programs, Fluid Running.
First, it comes with an aqua jogging belt and waterpoof bluetooth headphones so you have everything you need to aqua jog effectively.
Second, they have an app that pairs with the headphones so you can get workouts, guided instructions on how to aqua jog properly, and motivation while you're actually pool running.
This has been an absolute game changer for me when I am injured.
I used to dread aqua jogging workouts because they were so boring and it took all my mental energy to stay consistent.
But, with workouts directly in my ear, it's changed the whole experience and I actually look forward to the workouts. So much so that I now use aqua jogging as a cross training activity in the summer, even when I am not injured.
Fluid running is an awesome deal when you consider it comes with the belt (highly recommended for better form), the waterproof headphones (game changer for making pool workouts fun), a tether (to add variety to the workouts you can do) and the guided workout app (to make your cross training structure and a whole lot more interesting).
That's why we've partnered with them to give you 2 additional running-specific workouts you can load into the app when you use the code RTTT .
Check out the product here and then on the checkout page, add the code RTTT in the coupon field and the workouts will be added to your order for free.
If you'd rather do the aqua jogging workouts on your own, here are some great ideas to get you started!
Medium Effort Workouts
The Pyramid
10 minutes easy warm up - 1:00 hard, 30 seconds easy - 1:30 hard, 30 seconds easy - 2:00 hard, 30 seconds easy - 2:30 hard, 30 seconds easy, go to 5:00 in 30 second intervals and then come back down the pyramid (4:30 hard, 30 easy, 4:00 hard, 30 easy etc). Finish with 10 minutes easy cool down.
Wave your hands in the air like you just don’t care
10 minutes easy warm up, 1 minute medium (87-92% of maximum heart rate or what feels like tempo effort), 1 minute sprint (95-100% of maximum heart rate or all out sprint), 30 seconds hands in air (keep moving your legs in the running motion, but put your hand above your head), 1 minute rest, Repeat 10-15 times. 10 minutes easy cool down.
Hard Workouts
One of the difficulties of cross training is replicating those truly lung-busting, difficult workouts.
So, if you’re going to be pool running quite a bit due to injury or limited training volume, invest in a bungee cord designed for sprinters.
Tie one end of the resistance band to a sturdy object (pole, lifeguard stand, pool ladder) and bring the other into the water with you.
Put the strap around your waist and begin aqua jog away from your starting point.
You’ll begin to notice the bungee tighten and resist against you (depending on the length of your pool, you may need to wrap the bungee around the supporting object or tie it in knots to make it shorter to feel resistance).
Spend a few moments testing yourself to see how far you can pull the bungee.
This is a great challenge and a fun way to compete with yourself during an otherwise boring cross training activity.
Now for the hard part:
Pick a point on the pool wall or side of the pool that you feel stretches the bungee to a very hard sprint that you could maintain for 60-90 seconds.
This will be your “sprint” marker that you’ll use on sprint intervals (95-100% of maximum heart rate or all out sprint).
Now:
Find a point that feels like the end of a hard tempo run.
Mark this spot as your “medium” interval distance.
When you complete the hard workouts, you can use these reference points to ensure that you maintain a very hard effort.
The springboard
10 minutes easy warm up, 90 seconds easy (slowly moving out and stretching the bungee), 2 minute medium, 1 minute sprint, 1 min rest (let the bungee pull you back – this is kind of fun). Repeat 10 times. 10 minutes easy cool down.
The race simulation
10 minutes easy warm up, 90 seconds easy (slowly moving out and stretching the bungee), 5 minutes medium (focus and concentrate, just like during the hard part of a race), 30 seconds sprint, 2 minutes rest. Repeat 4 times. 10 minutes easy col down
The lactic acid
10 minutes easy warm up, 90 seconds easy (slowly moving out and stretching the bungee), 2 minutes sprint, 90 seconds rest. Repeat 12 times, 10 minutes easy cool down.
I guarantee that with the bungee, you’ll get your heart rate through the roof.
You can challenge yourself and make aqua jogging more fun by seeing how long you can stay at your maximum stretched distance or seeing how far you can push it.
Likewise, if you have a friend who is injured (or someone willing to be a good sport) you can try pulling each other across the pool for some competitive fun.
Cross training can be tough, especially when you’re injured or want to be increasing your volume faster.
However, I hope that providing a variety of workouts, either through the Fluid Running app (which also makes it easier to keep track of the workout while in the water) or on your own can add a fun challenge in the pool and you can emerge from your injury with minimal fitness loss.
Return To Running
Since piriformis syndrome is so poorly studied in runners, there aren’t any good return to running programs that have been scientifically validated. Still, as your hip strength improves, you can see how your piriformis reacts to running.
You’ll likely find that your tolerance for distance and speed increases linearly along with your hip strength. As with most injuries, no pain is a lot of gain.
You can carefully and gradually work your way back towards your usual running routine. But be aware that it can take several weeks for a hip strengthening program to fully kick in. Even when you are doing the stretches and strengthening exercises every day.