
Sharp pains along the inner part of your foot or ankle. Visible inflammation along the tendon. Stiffness in your ankle joint. A popping sensation. Sore to the touch.
Do any of those sound familiar?
If so, you probably have Posterior Tibial Tendon Dysfunction (Posterior Tibial Tendonitis).
In this article, I’m going to show you the exact steps to overcome this injury and get back to running strong again.
How Do You Diagnose, Treat and Prevent?
You are probably at the point where running is almost impossible. It hurts all the time, and even after you tried to run through it, hoping it would go away, you have come to the realization that maybe it is time to admit defeat and get it taken care of.
We have been there. It will stop training in its tracks, and you wonder if you will ever run pain free again.
Fortunately, we have the solution.
We have put together a guide to help you return to running as quickly as possible, and prevent this from coming back in the future.
About Posterior Tibial Tendonitis
- General introduction to the injury. Commonness, frequency, etc.
- Signs and symptoms
- Anatomy – use anatomy charts to pinpoint exact areas
The posterior tibial tendon is a little-known, but hugely important anatomical structure along the inside of your ankle. The tendon itself is not much thicker than a pencil, but it plays an essential role in stabilizing your foot.
The posterior tibial tendon inserts into your foot along your instep, runs up beside the medial malleolus. The large bump on the inside of your ankle and attaches to the tibialis posterior muscle, which is buried deep inside your calves.
By applying tension along the inside of your ankle, the tibialis posterior muscle and the posterior tibial tendon play a critical role in maintaining your arch and supporting your foot.
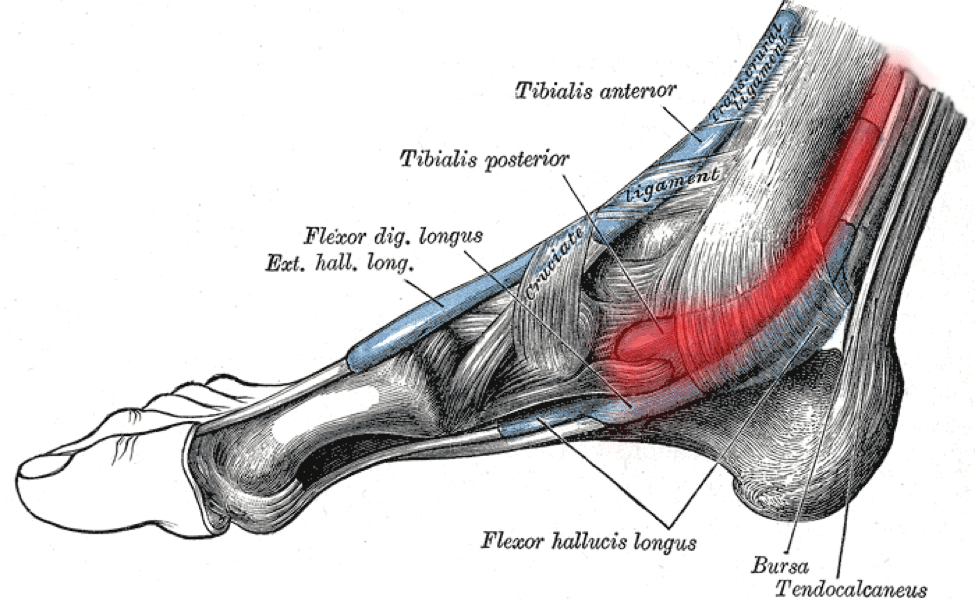
Any time you run or walk, your posterior tibial tendon locks your ankle in place, helping to hold your foot in a strong, rigid configuration when you push off the ground. It also functions to invert your foot, rolling your ankle to shift your weight to the outside of your foot.
The hallmark sign of posterior tibial tendon dysfunction is localized pain along the inside of your foot and ankle, sometimes stretching up a few inches onto your shin. There might be some mild swelling around the tendon, and the area might be tender or painful if you push on it. You may experience pain when you try to activate your posterior tibial tendon by lifting the inside of your foot off the ground, but the best diagnostic test is the single-leg heel raise.
Stand on the affected foot with your knee locked straight, and use your calf muscles to rise up all the way onto your forefoot, locking your ankle into full plantarflexion at the top.
Does this cause pain along the inside of your ankle or foot? If so, you probably have posterior tibial tendon dysfunction.
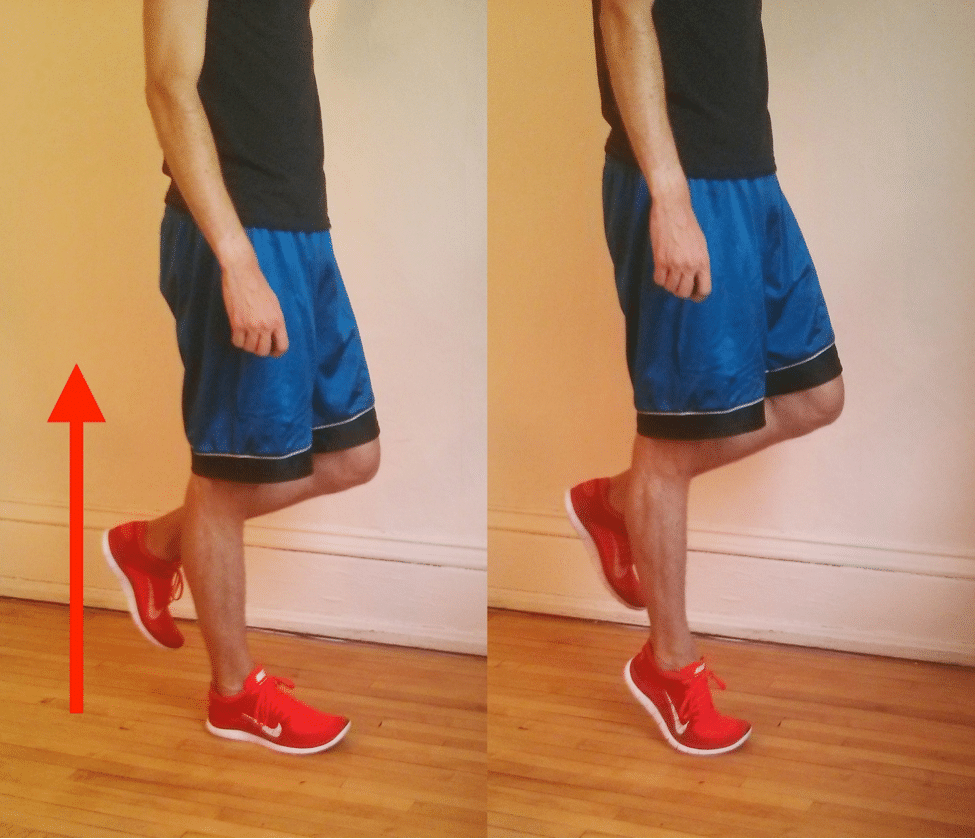
This might seem confusing—why would a calf exercise provoke pain along the posterior tibial tendon?
The answer lies in the posterior tibial tendon’s role as a stabilizer of the foot.
If the arch of your foot is like a suspension bridge, the posterior tibial tendon is the huge steel cable that provides the tension to support it. Without a strong, properly functioning posterior tibial tendon, your arch can’t stay up, your ankle can’t stay locked, and your calves can’t leverage their strength across the joints in your foot.
People with severe cases of posterior tibial tendon dysfunction can barely get their heel off the ground.
The single-leg heel raise is useful enough that some research articles use it as an inclusion criteria for patients in their studies.
It is also very helpful for ruling out other injuries that can cause pain in the same area, like medial tibial stress syndrome (shin splints) or a stress fracture of the medial malleolus.
What Is Happening? Am I Making It Worse?
Though it’s not a well-known running injury—only the 26th most common injury, according to one study1—posterior tibial tendon dysfunction (sometimes also called posterior tibial tendonitis) can be extremely difficult to get rid of.
Worse, if not addressed, it has the tendency to become progressively worse over time. In some cases, it can become so severe that your foot’s arch collapses, leaving you with a permanently deformed foot.
It gets worse:
As posterior tibial tendon dysfunction worsens, your arch height drops and your foot becomes more pronated when you put weight on it because the tendon can no longer provide adequate support.
As a result, the tension on the posterior tibial tendon increases. This creates a vicious cycle where a lower arch and increased pronation increase stress on the posterior tibial tendon, which in turn sustains more damage, leading to even greater arch collapse and pronation, and the cycle starts again.2
Why Did This Happen?
Because of the relative rarity of posterior tibial tendon dysfunction, especially among runners, its causal factors are poorly understood. However, common causes of this injury are due to overuse (such as too much running, too quickly or too soon) or an acute tear due to a fall.
Some researchers, like Melissa Rabbito and colleagues at the University of Calgary, have hypothesized that having a naturally high arch is protective against posterior tibial tendon dysfunction, but it’s possible for runners of all arch heights to wind up with this injury.2
Beyond this, it’s unclear what puts you at risk for posterior tibial tendon dysfunction. Among the general population, it’s most common among overweight, middle-aged women, but this doesn’t give any insight into runners. Even the role of gender is not clear.
While posterior tibial tendon dysfunction is more common among women in the general population, a 2002 review of over two thousand injured runners found eight men with posterior tibial tendon dysfunction, but only three women.1
Stages Of Severity
Doctors categorize posterior tibial tendon dysfunction into four stages:
- Stage I features tendon damage or inflammation, but no change in foot shape.
- Stage II, the tendon begins to become elongated, and the arch gradually flattens. Once in this phase, you probably will not be able to perform a single-leg heel raise at all.
- Stages III and IV, the tendon may be partially or fully ruptured, and there are permanent deformities in your foot and ankle.3
Research Backed Treatment Options
Because of the progressive and degenerative nature of posterior tibial tendon dysfunction, your first order of business should be to make sure you’re not doing any permanent damage.
You should see a podiatrist or foot and ankle orthopedist who has experience working with runners to make sure you’re still in stage I—the treatments discussed here could be injurious if you are in stage II or beyond. These cases often require specialized orthotic braces that fit over your ankle and foot to offload your posterior tibial tendon, and stages III and IV usually require surgery.
Fortunately, there are a number of scientific studies which have demonstrated that it is possible to successfully treat posterior tibial tendon dysfunction with conservative measures.
From these, it becomes clear that there should be four key components to your recovery program: Reducing stress on the tendon, using a corrective orthotic, stretching of the lower leg, and strengthening the surrounding area.

Sharp pains along the inner part of your foot or ankle. Visible inflammation along the tendon. Stiffness in your ankle joint. A popping sensation. Sore to the touch.
Do any of those sound familiar?
If so, you probably have Posterior Tibial Tendon Dysfunction (Posterior Tibial Tendonitis).
In this article, I’m going to show you the exact steps to overcome this injury and get back to running strong again.
How Do You Diagnose, Treat and Prevent?
You are probably at the point where running is almost impossible. It hurts all the time, and even after you tried to run through it, hoping it would go away, you have come to the realization that maybe it is time to admit defeat and get it taken care of.
We have been there. It will stop training in its tracks, and you wonder if you will ever run pain free again.
Fortunately, we have the solution.
We have put together a guide to help you return to running as quickly as possible, and prevent this from coming back in the future.
About Posterior Tibial Tendonitis
- General introduction to the injury. Commonness, frequency, etc.
- Signs and symptoms
- Anatomy – use anatomy charts to pinpoint exact areas
The posterior tibial tendon is a little-known, but hugely important anatomical structure along the inside of your ankle. The tendon itself is not much thicker than a pencil, but it plays an essential role in stabilizing your foot.
The posterior tibial tendon inserts into your foot along your instep, runs up beside the medial malleolus. The large bump on the inside of your ankle and attaches to the tibialis posterior muscle, which is buried deep inside your calves.
By applying tension along the inside of your ankle, the tibialis posterior muscle and the posterior tibial tendon play a critical role in maintaining your arch and supporting your foot.
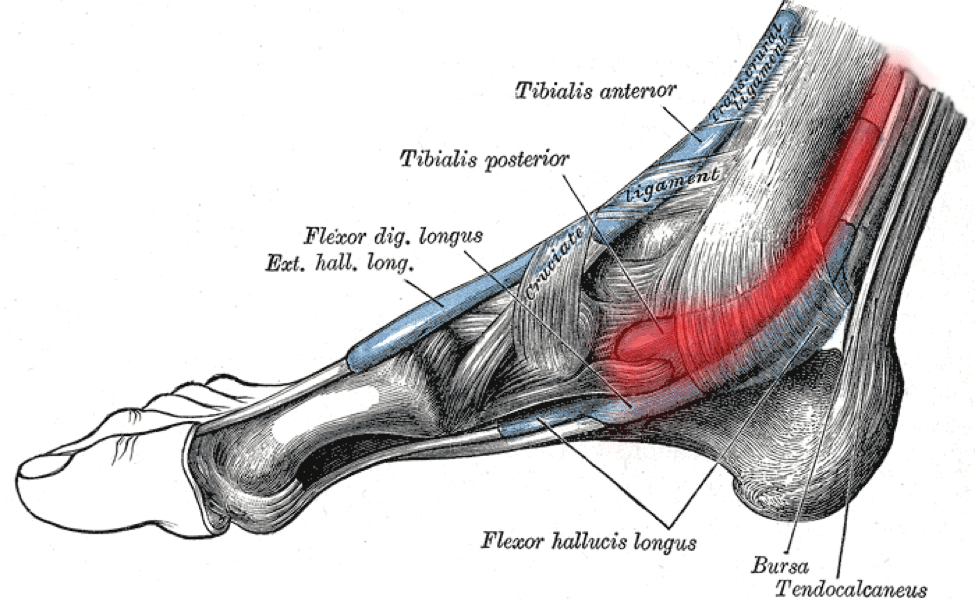
Any time you run or walk, your posterior tibial tendon locks your ankle in place, helping to hold your foot in a strong, rigid configuration when you push off the ground. It also functions to invert your foot, rolling your ankle to shift your weight to the outside of your foot.
The hallmark sign of posterior tibial tendon dysfunction is localized pain along the inside of your foot and ankle, sometimes stretching up a few inches onto your shin. There might be some mild swelling around the tendon, and the area might be tender or painful if you push on it. You may experience pain when you try to activate your posterior tibial tendon by lifting the inside of your foot off the ground, but the best diagnostic test is the single-leg heel raise.
Stand on the affected foot with your knee locked straight, and use your calf muscles to rise up all the way onto your forefoot, locking your ankle into full plantarflexion at the top.
Does this cause pain along the inside of your ankle or foot? If so, you probably have posterior tibial tendon dysfunction.
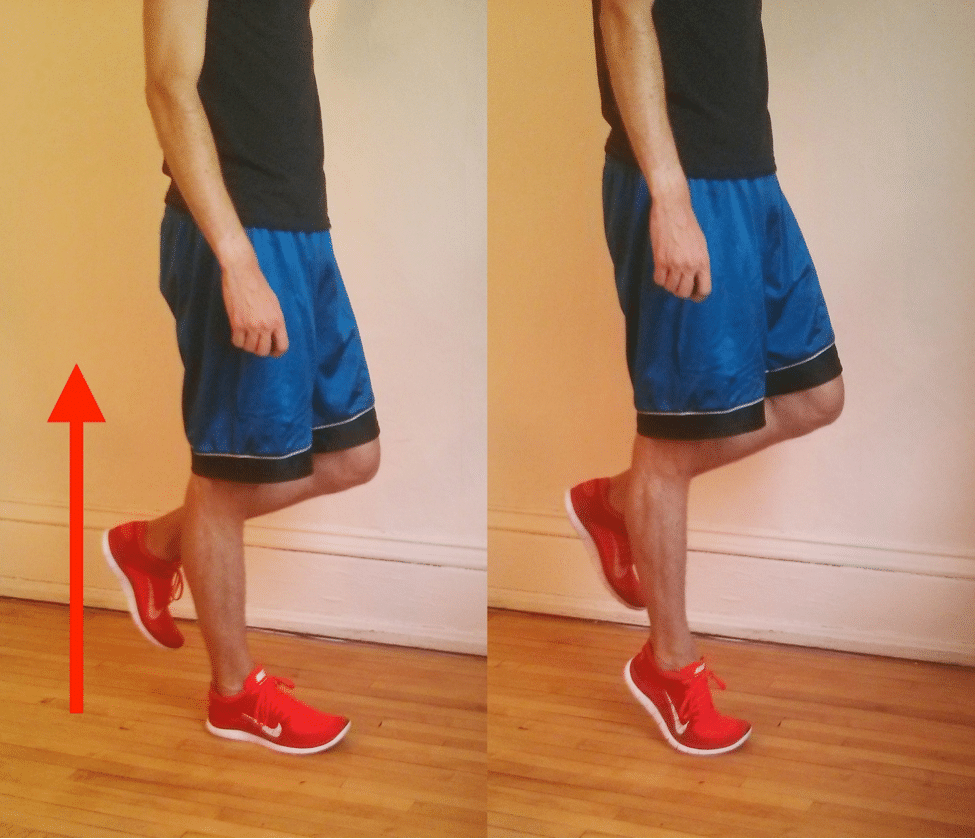
This might seem confusing—why would a calf exercise provoke pain along the posterior tibial tendon?
The answer lies in the posterior tibial tendon’s role as a stabilizer of the foot.
If the arch of your foot is like a suspension bridge, the posterior tibial tendon is the huge steel cable that provides the tension to support it. Without a strong, properly functioning posterior tibial tendon, your arch can’t stay up, your ankle can’t stay locked, and your calves can’t leverage their strength across the joints in your foot.
People with severe cases of posterior tibial tendon dysfunction can barely get their heel off the ground.
The single-leg heel raise is useful enough that some research articles use it as an inclusion criteria for patients in their studies.
It is also very helpful for ruling out other injuries that can cause pain in the same area, like medial tibial stress syndrome (shin splints) or a stress fracture of the medial malleolus.
What Is Happening? Am I Making It Worse?
Though it’s not a well-known running injury—only the 26th most common injury, according to one study1—posterior tibial tendon dysfunction (sometimes also called posterior tibial tendonitis) can be extremely difficult to get rid of.
Worse, if not addressed, it has the tendency to become progressively worse over time. In some cases, it can become so severe that your foot’s arch collapses, leaving you with a permanently deformed foot.
It gets worse:
As posterior tibial tendon dysfunction worsens, your arch height drops and your foot becomes more pronated when you put weight on it because the tendon can no longer provide adequate support.
As a result, the tension on the posterior tibial tendon increases. This creates a vicious cycle where a lower arch and increased pronation increase stress on the posterior tibial tendon, which in turn sustains more damage, leading to even greater arch collapse and pronation, and the cycle starts again.2
Why Did This Happen?
Because of the relative rarity of posterior tibial tendon dysfunction, especially among runners, its causal factors are poorly understood. However, common causes of this injury are due to overuse (such as too much running, too quickly or too soon) or an acute tear due to a fall.
Some researchers, like Melissa Rabbito and colleagues at the University of Calgary, have hypothesized that having a naturally high arch is protective against posterior tibial tendon dysfunction, but it’s possible for runners of all arch heights to wind up with this injury.2
Beyond this, it’s unclear what puts you at risk for posterior tibial tendon dysfunction. Among the general population, it’s most common among overweight, middle-aged women, but this doesn’t give any insight into runners. Even the role of gender is not clear.
While posterior tibial tendon dysfunction is more common among women in the general population, a 2002 review of over two thousand injured runners found eight men with posterior tibial tendon dysfunction, but only three women.1
Stages Of Severity
Doctors categorize posterior tibial tendon dysfunction into four stages:
- Stage I features tendon damage or inflammation, but no change in foot shape.
- Stage II, the tendon begins to become elongated, and the arch gradually flattens. Once in this phase, you probably will not be able to perform a single-leg heel raise at all.
- Stages III and IV, the tendon may be partially or fully ruptured, and there are permanent deformities in your foot and ankle.3
Research Backed Treatment Options
Because of the progressive and degenerative nature of posterior tibial tendon dysfunction, your first order of business should be to make sure you’re not doing any permanent damage.
You should see a podiatrist or foot and ankle orthopedist who has experience working with runners to make sure you’re still in stage I—the treatments discussed here could be injurious if you are in stage II or beyond. These cases often require specialized orthotic braces that fit over your ankle and foot to offload your posterior tibial tendon, and stages III and IV usually require surgery.
Fortunately, there are a number of scientific studies which have demonstrated that it is possible to successfully treat posterior tibial tendon dysfunction with conservative measures.
From these, it becomes clear that there should be four key components to your recovery program: Reducing stress on the tendon, using a corrective orthotic, stretching of the lower leg, and strengthening the surrounding area.
RunnersConnect Bonus
Download our Posterior Tibial Injury Outline for free.
It’s a PDF with the conservative and aggressive treatment options for runners suffering from Posterior tibial tendon pain
Reducing The Stress On Your Posterior Tibial Tendon
If you were trying to run through this injury, stop!
It’s not worth risking permanent damage to your arch. The posterior tibial tendon is slow to heal; probably because the portion of the tendon which runs along the medial malleolus has poor blood supply.4
Therefore, you should take plenty of time off and try to cut back on other activities that aggravate your tendon. Cross training activities like swimming and biking are okay as long as they don’t cause pain.5
We know that is not what you want to hear, but you could be putting yourself out for a long time if you continue to train through it. We have shown in previous articles that you can race well off cross training, and you can maintain conditioning for up to six weeks of no running.
A Podcast With Alan Webb, Elliptigo And Lynda Huey
7 ways cross training will make you a stronger and better runner.
Using Supportive Shoes And Orthotics
This also has the goal of reducing stress on the tendon.
All of the scientific studies in the literature use custom-made orthotics to provide extra arch support, which reduces the demands on the posterior tibial tendon.6, 7, 5
In one study, participants were asked to wear shoes and orthotics for at least 90% of their waking hours for the study’s six-month duration.6 In other research on running injuries where orthotics have proven useful, like plantar fasciitis, rigid over-the-counter orthotics like SuperFeet or PowerStep have been found to be just as useful as custom-made ones.8, 9
In the case of posterior tibial tendon dysfunction, however, there’s no research to support this. All we can say is that you should definitely be in some kind of supportive orthotic; whether or not you can use an over-the-counter orthotic is a question you should ask your orthopedist or podiatrist.

Calf Stretching
Three separate studies which successfully treated posterior tibial tendon dysfunction with conservative measures all employed a calf stretching regimen.7, 6, 5 The standard stretching protocol is 3×30 seconds of a standing calf stretch against a wall, both with a straight knee and a bent knee, done twice a day.
You should stretch both sides, and if you have an incline board, you should use it to get a better stretch. A 2009 study by Kornelia Kulig and colleagues at the University of Southern California emphasizes that you should be wearing your shoes and orthotics while doing your stretches.6
Strengthening Exercises For The Posterior Tibial Tendon
A 2006 paper by Richard Alvarez and a team of doctors and physical therapists at the University of Tennessee College of Medicine lays out a comprehensive rehab program for stage I posterior tibial tendon dysfunction.5
Alvarez et al.’s program contains two phases. In the first phase, rehab exercises address basic muscular endurance through a seated “sole to sole” exercise and three theraband exercises: inversion, eversion, and dorsiflexion.
These exercises are done with only light resistance, aiming for a large number of repetitions. The seated sole to sole exercise should begin with 4 sets of 25 repeats every day, building up to 12 sets of 25 by two weeks into the rehab program. Thereafter, you should combine sets until you can do 300 repeats continuously without a break.
Now:
The three theraband exercises—inversion, eversion, and dorsiflexion—are also done once per day. Alvarez et al. recommend doing 200 repeats, starting with a very weak theraband, and taking breaks if needed. Eventually you should progress towards doing them continuously.
Once you can do 200 repeats comfortably, you should move to a stronger theraband. Putting a towel under your foot allows for a smoother motion, and keeping the theraband at 45 degrees for the inversion and eversion exercises ensures you engage the right muscles. Take care not to rotate your leg while doing the theraband exercises; all of the motion should come from your ankle.
All of the theraband exercises should be done in shoes and orthotics. Make sure you do both the “up” and “down” portions of the exercises slowly.
Two papers by Kulig et al. used a specially-designed machine to eccentrically strengthen the posterior tibial tendon, but the authors suggest that Alvarez et al.’s foot inversion theraband exercise could function as a possible replacement.7, 6 Kulig et al.’s study called for more resistance, though—three sets of 15 repeats of the inversion exercise at the highest tolerable resistance, done twice per day.
It probably makes sense to take both approaches, using Alvarez et al.’s three high-rep theraband exercises once per day to build endurance, and Kulig et al.’s 3×15 twice-daily program for the inversion exercise with a stronger theraband to build strength.
But Wait! There’s more!
In the second phase of Alvarez et al.’s program, which begins after three weeks of the first phase, single-leg heel raises, toe walking, and balance board work is added in to begin using the posterior tibial tendon in a more functional way.
The single leg heel raise is exactly the same as the diagnostic test.
Stand on one leg and slowly rise up as high as possible, putting your hands lightly against a wall for balance if needed. Lower yourself down in a slow and controlled fashion. Start with only a few heel raises, and progress over time until you can get to 50 single leg heel raises. Like with the theraband exercises, wear your shoes and orthotics while doing heel raises.
Toe walking is fairly simple: walk forward with your ankles plantarflexed, keeping your heels high above the ground. Start with only 8 or 10 yards, and slowly progress over time until you can toe-walk for 100 yards.
Almost there!
Finally, Alvarez et al.’s program calls for balance board training with “tapping” in five different directions.
While standing on the affected leg on a balance board, “tap” the board to the ground and return to a balanced position 20 times each for all five of the positions illustrated in the photo. Then repeat going the opposite direction (e.g. progressing clockwise instead of counter-clockwise).
This brings the total to two sets of 20 repeats for each direction.
For all rehab exercises with this injury, you should stop if you have cause any significant pain. Unlike some other tendon injuries, pushing into pain is not a good idea here!
Alvarez et al.’s rehab program lasted for sixteen weeks (including a two week rest period before starting rehab exercises), and Kulig et al.’s rehab programs lasted for ten or twelve weeks, so you should plan on doing these exercises on a daily basis for at least three months.
Other Possible Treatment Options
Since posterior tibial tendon dysfunction is so sparsely researched, there is not much information on additional treatments. Icing often (especially after doing your rehab exercises) is strongly recommended, both by runners and in the scientific literature.5 Foam rolling your calf muscles should help too, since loosening your calves up will reduce stress on your posterior tibial tendon.
If these general exercises aren’t helping, you might want to see a physical therapist who can identify whether you have any other strength or flexibility deficits that are contributing to your posterior tibial tendon dysfunction.
What’s the bottom line?
If you still haven’t improved after several months of conservative treatment, you should consult with a trusted podiatrist or orthopedist and discuss the possibility of surgery. There are dozens of different surgical techniques to attempt to repair a damaged or ruptured posterior tibial tendon, so it definitely pays off to see a doctor with a lot of experience.
Conservative Treatment Options
Methods that are fairly simple, inexpensive, and can be done on your own at home.
- Wear supportive shoes and orthotics all the time, even when you’re just walking around the house. Talk with your doctor or podiatrist about whether you can use a rigid over-the-counter orthotic or if you need a custom-made orthotic.
- Calf stretching, 3×30 seconds, both with a straight knee and bent knee, on both legs, twice per day. Use an incline board if you have one.
- Seated sole to sole exercise, once per day. Start with 4 sets of 25 repeats every day and build up to 12 sets of 25 after two weeks. Thereafter, begin combining sets until you can do 300 repeats continuously without a break.
- Theraband exercises, once per day (except 4).For the first three exercises, progress to a stronger theraband once you can comfortably do all 200 repeats without any breaks.
- Dorsiflexion, 200 repeats. Use a towel to decrease friction under your foot.
- Inversion, 200 repeats. Use a towel to decrease friction under your foot and position the theraband at 45 degrees.
- Eversion, 200 repeats. Use a towel to decrease friction under your foot and position the theraband at 45 degrees.
- Inversion, 3 sets of 15 repeats with as much resistance as you can comfortably tolerate. Do this twice per day and increase resistance over time. Use a towel to decrease friction under your foot and position the theraband at 45 degrees.
- Functional exercises, done once per day. To be added once you have been doing steps 3 and 4 for at least three weeks.
- Single leg heel raise, building up gradually to 50 repeats
- Toe walking, starting at 8-10 yards and building up to 100 yards of continuous toe walking
- Balance board tapping: On a balance board, “tap” the board to the ground and return to a balanced position 20 times each for all five of the positions illustrated in the photo. Then repeat going the opposite direction for a total of two sets of 20 taps for each direction.
- Ice to control pain, especially after doing your rehab exercises. Try 10 minutes of ice massage with an ice cup, followed by a 10 minute rest, and finally another 10 minutes of icing. You can ice as often as every two hours.
Aggressive Treatment Options
These are treatments with more cost and less certainty about outcomes, but may prove useful in recalcitrant cases.
- Custom orthotics from a podiatrist or foot and ankle orthopedist. Although these can be expensive and not all insurance companies cover them, your doctor may recommend them to provide better support for your foot.
- See a physical therapist to get a personalized rehab program and discuss other non-invasive treatments.
- See a trusted orthopedist or podiatrist to discuss the possibility of surgery.
Cross Training While Injured and During Recovery
Cross training is recommended while you’re injured and as you slowly return to running.
The best form of cross training for this injury is Aqua Jogging. Studies have shown that aqua jogging can enable a well-trained runner to maintain running fitness for up to 4-6 weeks.
Aqua jogging is a form of deep water running that closely mimics the actual running movement. Your feet don’t actually touch the bottom of the pool, so it is zero impact and safe for almost any type of injury. In my experience, the only time to avoid aqua jogging is when you have a hip flexor injury, which can be aggravated by the increased resistance of the water as you bring your leg up. Because aqua jogging closely mimics natural running form, it provides a neuromuscular workout that, in addition to aerobic benefits, helps keep the running specific muscles active. The same can’t be said for biking and swimming. The only downside to aqua jogging is that you need a pool that is deep enough to run in without touching the bottom. If you’re lucky enough to have access to a pool of this size, aqua jogging should be your first cross training choice.In one study, a group of ten runners trained exclusively with deep water running for four weeks and compared 5km race times pre deep water running and post deep water running.
The researchers found no statistical difference in 5k time or other markers for performance, such as submaximal oxygen consumption or lactate threshold.
In a second study, researchers measured the effects of aqua jogging over a six week period.
This time, 16 runners were separated into two groups – one who did aqua jogging workouts and the other who did over land running.
Using the same training intensities and durations, the researchers found no difference between the groups in maximal blood glucose, blood lactate, and body composition.
It get’s better:
Research has also demonstrated that aqua jogging can be used as a recovery tool to facilitate the repair of damaged muscles after hard workouts.
These findings make aqua jogging an important recovery tool in addition to being the best cross training method for injuries.
Need one more reason?
The calories burned aqua jogging are even higher than running on land, so if you want to avoid weight gain while you take time off from running, this is definitely the exercise for you!
Aqua Jogging Workouts For Runners
If you’re interested in aqua jogging to rehab your injury, then the absolute best way is to use one of my favorite programs, Fluid Running.
First, it comes with an aqua jogging belt and waterpoof bluetooth headphones so you have everything you need to aqua jog effectively.
Second, they have an app that pairs with the headphones so you can get workouts, guided instructions on how to aqua jog properly, and motivation while you’re actually pool running.
This has been an absolute game changer for me when I am injured.
I used to dread aqua jogging workouts because they were so boring and it took all my mental energy to stay consistent.
But, with workouts directly in my ear, it’s changed the whole experience and I actually look forward to the workouts. So much so that I now use aqua jogging as a cross training activity in the summer, even when I am not injured.
Fluid running is an awesome deal when you consider it comes with the belt (highly recommended for better form), the waterproof headphones (game changer for making pool workouts fun), a tether (to add variety to the workouts you can do) and the guided workout app (to make your cross training structure and a whole lot more interesting).
That’s why we’ve partnered with them to give you 2 additional running-specific workouts you can load into the app when you use the code RTTT .
Check out the product here and then on the checkout page, add the code RTTT in the coupon field and the workouts will be added to your order for free.
If you’d rather do the aqua jogging workouts on your own, here are some great ideas to get you started!
Medium Effort Workouts
The Pyramid
10 minutes easy warm up – 1:00 hard, 30 seconds easy – 1:30 hard, 30 seconds easy – 2:00 hard, 30 seconds easy – 2:30 hard, 30 seconds easy, go to 5:00 in 30 second intervals and then come back down the pyramid (4:30 hard, 30 easy, 4:00 hard, 30 easy etc). Finish with 10 minutes easy cool down.
Wave your hands in the air like you just don’t care
10 minutes easy warm up, 1 minute medium (87-92% of maximum heart rate or what feels like tempo effort), 1 minute sprint (95-100% of maximum heart rate or all out sprint), 30 seconds hands in air (keep moving your legs in the running motion, but put your hand above your head), 1 minute rest, Repeat 10-15 times. 10 minutes easy cool down.
Hard Workouts
One of the difficulties of cross training is replicating those truly lung-busting, difficult workouts.
So, if you’re going to be pool running quite a bit due to injury or limited training volume, invest in a bungee cord designed for sprinters.
Tie one end of the resistance band to a sturdy object (pole, lifeguard stand, pool ladder) and bring the other into the water with you.
Put the strap around your waist and begin aqua jog away from your starting point.
You’ll begin to notice the bungee tighten and resist against you (depending on the length of your pool, you may need to wrap the bungee around the supporting object or tie it in knots to make it shorter to feel resistance).
Spend a few moments testing yourself to see how far you can pull the bungee.
This is a great challenge and a fun way to compete with yourself during an otherwise boring cross training activity.
Now for the hard part:
Pick a point on the pool wall or side of the pool that you feel stretches the bungee to a very hard sprint that you could maintain for 60-90 seconds.
This will be your “sprint” marker that you’ll use on sprint intervals (95-100% of maximum heart rate or all out sprint).
Now:
Find a point that feels like the end of a hard tempo run.
Mark this spot as your “medium” interval distance.
When you complete the hard workouts, you can use these reference points to ensure that you maintain a very hard effort.
The springboard
10 minutes easy warm up, 90 seconds easy (slowly moving out and stretching the bungee), 2 minute medium, 1 minute sprint, 1 min rest (let the bungee pull you back – this is kind of fun). Repeat 10 times. 10 minutes easy cool down.
The race simulation
10 minutes easy warm up, 90 seconds easy (slowly moving out and stretching the bungee), 5 minutes medium (focus and concentrate, just like during the hard part of a race), 30 seconds sprint, 2 minutes rest. Repeat 4 times. 10 minutes easy col down
The lactic acid
10 minutes easy warm up, 90 seconds easy (slowly moving out and stretching the bungee), 2 minutes sprint, 90 seconds rest. Repeat 12 times, 10 minutes easy cool down.
I guarantee that with the bungee, you’ll get your heart rate through the roof.
You can challenge yourself and make aqua jogging more fun by seeing how long you can stay at your maximum stretched distance or seeing how far you can push it.
Likewise, if you have a friend who is injured (or someone willing to be a good sport) you can try pulling each other across the pool for some competitive fun.
Cross training can be tough, especially when you’re injured or want to be increasing your volume faster.
However, I hope that providing a variety of workouts, either through the Fluid Running app (which also makes it easier to keep track of the workout while in the water) or on your own can add a fun challenge in the pool and you can emerge from your injury with minimal fitness loss.
Return To Running
Since posterior tibial tendon dysfunction has such a reputation for causing permanent damage if it’s not properly taken care of, you should be very gradual when you return to running.
No scientific research has offered any advice on return-to-running plans, but you should be very cautious, starting out with only small amounts of easy jogging and returning slowly to training, backing off if you have any pain. A physical therapist with experience working with distance runners can help you develop an individualized program if needed.
Reducing The Stress On Your Posterior Tibial Tendon
If you were trying to run through this injury, stop!
It’s not worth risking permanent damage to your arch. The posterior tibial tendon is slow to heal; probably because the portion of the tendon which runs along the medial malleolus has poor blood supply.4
Therefore, you should take plenty of time off and try to cut back on other activities that aggravate your tendon. Cross training activities like swimming and biking are okay as long as they don’t cause pain.5
We know that is not what you want to hear, but you could be putting yourself out for a long time if you continue to train through it. We have shown in previous articles that you can race well off cross training, and you can maintain conditioning for up to six weeks of no running.
A Podcast With Alan Webb, Elliptigo And Lynda Huey
7 ways cross training will make you a stronger and better runner.
Using Supportive Shoes And Orthotics
This also has the goal of reducing stress on the tendon.
All of the scientific studies in the literature use custom-made orthotics to provide extra arch support, which reduces the demands on the posterior tibial tendon.6, 7, 5
In one study, participants were asked to wear shoes and orthotics for at least 90% of their waking hours for the study’s six-month duration.6 In other research on running injuries where orthotics have proven useful, like plantar fasciitis, rigid over-the-counter orthotics like SuperFeet or PowerStep have been found to be just as useful as custom-made ones.8, 9
In the case of posterior tibial tendon dysfunction, however, there’s no research to support this. All we can say is that you should definitely be in some kind of supportive orthotic; whether or not you can use an over-the-counter orthotic is a question you should ask your orthopedist or podiatrist.

Calf Stretching
Three separate studies which successfully treated posterior tibial tendon dysfunction with conservative measures all employed a calf stretching regimen.7, 6, 5 The standard stretching protocol is 3×30 seconds of a standing calf stretch against a wall, both with a straight knee and a bent knee, done twice a day.
You should stretch both sides, and if you have an incline board, you should use it to get a better stretch. A 2009 study by Kornelia Kulig and colleagues at the University of Southern California emphasizes that you should be wearing your shoes and orthotics while doing your stretches.6
Strengthening Exercises For The Posterior Tibial Tendon
A 2006 paper by Richard Alvarez and a team of doctors and physical therapists at the University of Tennessee College of Medicine lays out a comprehensive rehab program for stage I posterior tibial tendon dysfunction.5
Alvarez et al.’s program contains two phases. In the first phase, rehab exercises address basic muscular endurance through a seated “sole to sole” exercise and three theraband exercises: inversion, eversion, and dorsiflexion.
These exercises are done with only light resistance, aiming for a large number of repetitions. The seated sole to sole exercise should begin with 4 sets of 25 repeats every day, building up to 12 sets of 25 by two weeks into the rehab program. Thereafter, you should combine sets until you can do 300 repeats continuously without a break.
Now:
The three theraband exercises—inversion, eversion, and dorsiflexion—are also done once per day. Alvarez et al. recommend doing 200 repeats, starting with a very weak theraband, and taking breaks if needed. Eventually you should progress towards doing them continuously.
Once you can do 200 repeats comfortably, you should move to a stronger theraband. Putting a towel under your foot allows for a smoother motion, and keeping the theraband at 45 degrees for the inversion and eversion exercises ensures you engage the right muscles. Take care not to rotate your leg while doing the theraband exercises; all of the motion should come from your ankle.
All of the theraband exercises should be done in shoes and orthotics. Make sure you do both the “up” and “down” portions of the exercises slowly.
Two papers by Kulig et al. used a specially-designed machine to eccentrically strengthen the posterior tibial tendon, but the authors suggest that Alvarez et al.’s foot inversion theraband exercise could function as a possible replacement.7, 6 Kulig et al.’s study called for more resistance, though—three sets of 15 repeats of the inversion exercise at the highest tolerable resistance, done twice per day.
It probably makes sense to take both approaches, using Alvarez et al.’s three high-rep theraband exercises once per day to build endurance, and Kulig et al.’s 3×15 twice-daily program for the inversion exercise with a stronger theraband to build strength.
But Wait! There’s more!
In the second phase of Alvarez et al.’s program, which begins after three weeks of the first phase, single-leg heel raises, toe walking, and balance board work is added in to begin using the posterior tibial tendon in a more functional way.
The single leg heel raise is exactly the same as the diagnostic test.
Stand on one leg and slowly rise up as high as possible, putting your hands lightly against a wall for balance if needed. Lower yourself down in a slow and controlled fashion. Start with only a few heel raises, and progress over time until you can get to 50 single leg heel raises. Like with the theraband exercises, wear your shoes and orthotics while doing heel raises.
Toe walking is fairly simple: walk forward with your ankles plantarflexed, keeping your heels high above the ground. Start with only 8 or 10 yards, and slowly progress over time until you can toe-walk for 100 yards.
Almost there!
Finally, Alvarez et al.’s program calls for balance board training with “tapping” in five different directions.
While standing on the affected leg on a balance board, “tap” the board to the ground and return to a balanced position 20 times each for all five of the positions illustrated in the photo. Then repeat going the opposite direction (e.g. progressing clockwise instead of counter-clockwise).
This brings the total to two sets of 20 repeats for each direction.
For all rehab exercises with this injury, you should stop if you have cause any significant pain. Unlike some other tendon injuries, pushing into pain is not a good idea here!
Alvarez et al.’s rehab program lasted for sixteen weeks (including a two week rest period before starting rehab exercises), and Kulig et al.’s rehab programs lasted for ten or twelve weeks, so you should plan on doing these exercises on a daily basis for at least three months.
Other Possible Treatment Options
Since posterior tibial tendon dysfunction is so sparsely researched, there is not much information on additional treatments. Icing often (especially after doing your rehab exercises) is strongly recommended, both by runners and in the scientific literature.5 Foam rolling your calf muscles should help too, since loosening your calves up will reduce stress on your posterior tibial tendon.
If these general exercises aren’t helping, you might want to see a physical therapist who can identify whether you have any other strength or flexibility deficits that are contributing to your posterior tibial tendon dysfunction.
What’s the bottom line?
If you still haven’t improved after several months of conservative treatment, you should consult with a trusted podiatrist or orthopedist and discuss the possibility of surgery. There are dozens of different surgical techniques to attempt to repair a damaged or ruptured posterior tibial tendon, so it definitely pays off to see a doctor with a lot of experience.
Conservative Treatment Options
Methods that are fairly simple, inexpensive, and can be done on your own at home.
- Wear supportive shoes and orthotics all the time, even when you’re just walking around the house. Talk with your doctor or podiatrist about whether you can use a rigid over-the-counter orthotic or if you need a custom-made orthotic.
- Calf stretching, 3×30 seconds, both with a straight knee and bent knee, on both legs, twice per day. Use an incline board if you have one.
- Seated sole to sole exercise, once per day. Start with 4 sets of 25 repeats every day and build up to 12 sets of 25 after two weeks. Thereafter, begin combining sets until you can do 300 repeats continuously without a break.
- Theraband exercises, once per day (except 4).For the first three exercises, progress to a stronger theraband once you can comfortably do all 200 repeats without any breaks.
- Dorsiflexion, 200 repeats. Use a towel to decrease friction under your foot.
- Inversion, 200 repeats. Use a towel to decrease friction under your foot and position the theraband at 45 degrees.
- Eversion, 200 repeats. Use a towel to decrease friction under your foot and position the theraband at 45 degrees.
- Inversion, 3 sets of 15 repeats with as much resistance as you can comfortably tolerate. Do this twice per day and increase resistance over time. Use a towel to decrease friction under your foot and position the theraband at 45 degrees.
- Functional exercises, done once per day. To be added once you have been doing steps 3 and 4 for at least three weeks.
- Single leg heel raise, building up gradually to 50 repeats
- Toe walking, starting at 8-10 yards and building up to 100 yards of continuous toe walking
- Balance board tapping: On a balance board, “tap” the board to the ground and return to a balanced position 20 times each for all five of the positions illustrated in the photo. Then repeat going the opposite direction for a total of two sets of 20 taps for each direction.
- Ice to control pain, especially after doing your rehab exercises. Try 10 minutes of ice massage with an ice cup, followed by a 10 minute rest, and finally another 10 minutes of icing. You can ice as often as every two hours.
Aggressive Treatment Options
These are treatments with more cost and less certainty about outcomes, but may prove useful in recalcitrant cases.
- Custom orthotics from a podiatrist or foot and ankle orthopedist. Although these can be expensive and not all insurance companies cover them, your doctor may recommend them to provide better support for your foot.
- See a physical therapist to get a personalized rehab program and discuss other non-invasive treatments.
- See a trusted orthopedist or podiatrist to discuss the possibility of surgery.
Cross Training While Injured and During Recovery
Cross training is recommended while you’re injured and as you slowly return to running.
The best form of cross training for this injury is Aqua Jogging. Studies have shown that aqua jogging can enable a well-trained runner to maintain running fitness for up to 4-6 weeks.
Aqua jogging is a form of deep water running that closely mimics the actual running movement. Your feet don’t actually touch the bottom of the pool, so it is zero impact and safe for almost any type of injury. In my experience, the only time to avoid aqua jogging is when you have a hip flexor injury, which can be aggravated by the increased resistance of the water as you bring your leg up. Because aqua jogging closely mimics natural running form, it provides a neuromuscular workout that, in addition to aerobic benefits, helps keep the running specific muscles active. The same can’t be said for biking and swimming. The only downside to aqua jogging is that you need a pool that is deep enough to run in without touching the bottom. If you’re lucky enough to have access to a pool of this size, aqua jogging should be your first cross training choice.In one study, a group of ten runners trained exclusively with deep water running for four weeks and compared 5km race times pre deep water running and post deep water running.
The researchers found no statistical difference in 5k time or other markers for performance, such as submaximal oxygen consumption or lactate threshold.
In a second study, researchers measured the effects of aqua jogging over a six week period.
This time, 16 runners were separated into two groups – one who did aqua jogging workouts and the other who did over land running.
Using the same training intensities and durations, the researchers found no difference between the groups in maximal blood glucose, blood lactate, and body composition.
It get’s better:
Research has also demonstrated that aqua jogging can be used as a recovery tool to facilitate the repair of damaged muscles after hard workouts.
These findings make aqua jogging an important recovery tool in addition to being the best cross training method for injuries.
Need one more reason?
The calories burned aqua jogging are even higher than running on land, so if you want to avoid weight gain while you take time off from running, this is definitely the exercise for you!
Aqua Jogging Workouts For Runners
If you’re interested in aqua jogging to rehab your injury, then the absolute best way is to use one of my favorite programs, Fluid Running.
First, it comes with an aqua jogging belt and waterpoof bluetooth headphones so you have everything you need to aqua jog effectively.
Second, they have an app that pairs with the headphones so you can get workouts, guided instructions on how to aqua jog properly, and motivation while you’re actually pool running.
This has been an absolute game changer for me when I am injured.
I used to dread aqua jogging workouts because they were so boring and it took all my mental energy to stay consistent.
But, with workouts directly in my ear, it’s changed the whole experience and I actually look forward to the workouts. So much so that I now use aqua jogging as a cross training activity in the summer, even when I am not injured.
Fluid running is an awesome deal when you consider it comes with the belt (highly recommended for better form), the waterproof headphones (game changer for making pool workouts fun), a tether (to add variety to the workouts you can do) and the guided workout app (to make your cross training structure and a whole lot more interesting).
That’s why we’ve partnered with them to give you 2 additional running-specific workouts you can load into the app when you use the code RTTT .
Check out the product here and then on the checkout page, add the code RTTT in the coupon field and the workouts will be added to your order for free.
If you’d rather do the aqua jogging workouts on your own, here are some great ideas to get you started!
Medium Effort Workouts
The Pyramid
10 minutes easy warm up – 1:00 hard, 30 seconds easy – 1:30 hard, 30 seconds easy – 2:00 hard, 30 seconds easy – 2:30 hard, 30 seconds easy, go to 5:00 in 30 second intervals and then come back down the pyramid (4:30 hard, 30 easy, 4:00 hard, 30 easy etc). Finish with 10 minutes easy cool down.
Wave your hands in the air like you just don’t care
10 minutes easy warm up, 1 minute medium (87-92% of maximum heart rate or what feels like tempo effort), 1 minute sprint (95-100% of maximum heart rate or all out sprint), 30 seconds hands in air (keep moving your legs in the running motion, but put your hand above your head), 1 minute rest, Repeat 10-15 times. 10 minutes easy cool down.
Hard Workouts
One of the difficulties of cross training is replicating those truly lung-busting, difficult workouts.
So, if you’re going to be pool running quite a bit due to injury or limited training volume, invest in a bungee cord designed for sprinters.
Tie one end of the resistance band to a sturdy object (pole, lifeguard stand, pool ladder) and bring the other into the water with you.
Put the strap around your waist and begin aqua jog away from your starting point.
You’ll begin to notice the bungee tighten and resist against you (depending on the length of your pool, you may need to wrap the bungee around the supporting object or tie it in knots to make it shorter to feel resistance).
Spend a few moments testing yourself to see how far you can pull the bungee.
This is a great challenge and a fun way to compete with yourself during an otherwise boring cross training activity.
Now for the hard part:
Pick a point on the pool wall or side of the pool that you feel stretches the bungee to a very hard sprint that you could maintain for 60-90 seconds.
This will be your “sprint” marker that you’ll use on sprint intervals (95-100% of maximum heart rate or all out sprint).
Now:
Find a point that feels like the end of a hard tempo run.
Mark this spot as your “medium” interval distance.
When you complete the hard workouts, you can use these reference points to ensure that you maintain a very hard effort.
The springboard
10 minutes easy warm up, 90 seconds easy (slowly moving out and stretching the bungee), 2 minute medium, 1 minute sprint, 1 min rest (let the bungee pull you back – this is kind of fun). Repeat 10 times. 10 minutes easy cool down.
The race simulation
10 minutes easy warm up, 90 seconds easy (slowly moving out and stretching the bungee), 5 minutes medium (focus and concentrate, just like during the hard part of a race), 30 seconds sprint, 2 minutes rest. Repeat 4 times. 10 minutes easy col down
The lactic acid
10 minutes easy warm up, 90 seconds easy (slowly moving out and stretching the bungee), 2 minutes sprint, 90 seconds rest. Repeat 12 times, 10 minutes easy cool down.
I guarantee that with the bungee, you’ll get your heart rate through the roof.
You can challenge yourself and make aqua jogging more fun by seeing how long you can stay at your maximum stretched distance or seeing how far you can push it.
Likewise, if you have a friend who is injured (or someone willing to be a good sport) you can try pulling each other across the pool for some competitive fun.
Cross training can be tough, especially when you’re injured or want to be increasing your volume faster.
However, I hope that providing a variety of workouts, either through the Fluid Running app (which also makes it easier to keep track of the workout while in the water) or on your own can add a fun challenge in the pool and you can emerge from your injury with minimal fitness loss.
Return To Running
Since posterior tibial tendon dysfunction has such a reputation for causing permanent damage if it’s not properly taken care of, you should be very gradual when you return to running.
No scientific research has offered any advice on return-to-running plans, but you should be very cautious, starting out with only small amounts of easy jogging and returning slowly to training, backing off if you have any pain. A physical therapist with experience working with distance runners can help you develop an individualized program if needed.




18 Responses
I struggled with PTT for years, and it ultimately ended my collegiate career. I finally overcame it years later with a combination of orthotics, clamshell strengthening, topical anti inflammatories, and support shoes. But the key was finding a good self massage technique. Slowly rotating the foot while working my thumbs up the tendon and muscle behind the ankle bone and up the shin finally got everything to relax.
Thanks for sharing Stuart!
I enjoyed reading this article and i have developed this injury (that i have never had before,even from running on the treadmill,too fast for too long)..I cycle much more than running,because i was cycling between 16 and 32 miles everyday for work and.I changed my job to a local job and i wasn’t doing all the cycling mileage everyday and two weeks ago i used my turbo trainer on my bike and cycled at 22 mph for 20 mins doing this three times,so 1 hour cycling at 22 mph. That was enough to give me this injury for the first time .I have learnt more valuable lessons from doing too much exercise,too fast for too long!!!.Also look how quickly my fitness from cycling 16 to 32 miles everyday to only cycling 4 miles to work everyday dropped my fitness like a stone and that is why i have got this injury when i cycled for 1 hour at 22mph after six weeks of only cycling 4 miles a day.I am just going to rest,rest and more rest until this injury has gone and then have to build up my cycling fitness again.I can lift my left heel with a little soreness,so i guess i’m still ok to make a full recovery with rest over time,i hope so.Thanks Bruce
Mine is a longitudinal tear of the peroneal brevis tendon–the stabilizing tendon on the outside of the foot. Would these healing protocols work for me also? Thank you.
Hi Derrick, yes, many of the exercises we recommend throughout our posts are helpful for a variety of different injuries as they are strengthening all the muscles around the lower leg to prevent future injuries of all kinds. You may also want to check this one to out to make sure it is not weakness in your hip that is causing this injury https://runnersconnect.net/running-injury-prevention/the-relationship-between-hip-strength-and-running-injuries-the-latest-research/ Hope this helps!
Hi Coach Tina , I have PTT and a doc I went to see is recommending EPAT therapy. I don’t know of anyone that has done this so I am trying to get a perspective on this treatment to see if it worthwhile or not. I know it is relatively new ,but I dont want to waste $300.00 per treatment (3 are recommended) if it is just a scam treatment or hasn’t produced results for anyone else. Any advice you or anyone can offer me on this treatment ?
Thank you for this information on how to treat post. tib issues. For 8 months, I have been aching from what my new podiatrist thinks is an inflamed post. tib tendon being impinged by a talus that is rotated 40 or so degrees medically plus a torn, chronically sprained deep deltoid ligaments. I have tried two rounds of physical therapy totaling about 4 months, several injections including PRP and steroids, and significant reductions in my activity. It took me a few months to stop running entirely (I am obsessed running!). Finally I am non-weight-baring on my injured foot (just started week three of that). Do you have any conjectures on whether complete rest will finally help reduce my pain? I am also open to any additional advice you are willing to provide on how to treat this nagging injury. Finally, my advice for anyone with this injury is to stop running immediately.
Hi Katie. I realize it’s been a while since you posted. But I’m reaching out to you because I have the same problems. Are you available to chat on our similar conditions.? Mark
I, too, have been suffering from PTT for over 8 months. It has completely stopped my running. I kept thinking it was getting better so I would try to run again only to have it flare up but even worse. Now I am unable to run at all. I just completed 6 weeks of total rest, wearing an Aircast and using crutches. It did start to feel a little better but the swelling remains and the soreness is returning now that I am weight bearing again. Not sure what options that I have now other than surgery. I have found that few therapists understand this injury and more often than not they make the problem worse. I have been using topical anti inflammatory gel (Voltaren) but not sure it has made any difference. If anyone has any ideas let me know! This is a very frustrating injury and there is no quick fix, at least for me.
Hello, I am also suffering from this problem and my doctor advise is surgery. however the process seems worse then the problem it self.
i believe before going to these extreme one should try self healing. it is base on faith and the ability the body have to heal it self though faith in God.
As a follow up to my own post, it has now been 13 months dealing with this injury and it’s finally getting better. I am not running but I can now do all other activities with very little pain. I recently visited a great doctor at the Mayo Clinic. He is a sports orthopedic doctor. He talked to me about the Alfredson Protocol. Developed for Achilles injuries, it can be applied to this tendon. It focuses on strengthening the tendon while elongating it versus contraction exercises. It works. Google this. Respond if you’d like any more information. Good luck!
Hi, I don’t see a description of the “sole to sole” exercise. What is this?
Help! For 10 years I have had PTT issues. Dr. says that I no longer have a tendon-that it must have snapped. Who knows why. Not overweight and don’t really exercise or anything that would have strained it. I still have a high arch-always have. I wear orthotics and a brace. Sometimes I question the whole thing. This article talks about the foot becoming pronated and the arch falling. I have neither issue. I can’t stand on one foot on that foot and the foot is somewhat inward facing at the ankle. Going to go to a new doctor soon. This doctor made an Arizona brace for me, but come on! Who is going to wear that thing? It doesn’t even fit in a gym shoe and I have a professional job where I couldn’t wear gym shoes. Anyone ever hear of a PTT just snapping? Dr. says MRI shows that the tendon is missing. Anyone have any insight into a disappearing PTT? My issues seem different than the ones in the article and the comments.
Thank you for this informative post that finally revealed what I’ve been experiencing all these years. I’m not sure if I was born with this, but as a kid I would sometimes stretch after waking, and my foot would suddenly ‘lock’ with a sharp and intense pain. Only by pressing and rubbing the arch of my foot was I able to relax it. And I had no idea it’s related to the reason why my feet hurts after standing for long periods in the recent years. I’m gonna try those stretching exercises.
I may have early stage of this injury. My question is how do I know if it is posterior tibial tendonitis or the flexor hallucis longus? Are the treatments the same? When it first started I researched it a bit, started icing, and put my “good feet” arch supports in my work shoes. I plan on beginning this rehab regimen. Last thing I want is a flat arch!
Help please. i have ptti. my orthotic specialist has put a wedge in the medial forefoot region . Should it be placed in posterior(hindfoot,by calcaneus or forefoot?-
Dr Barry Shapiro
bps1@rogers.com
Chris said:
I’m in my 80’s, and although I’m not a runner I have been very active outdoors throughout my life. However, after a series of incidents since childhood, I now realize that earlier diagnoses as Plantar Fasciitis were hasty and incorrect, and that what I really have is Posterior Tibial Tendonitis! Now, I’m very pleased to have this information and the treatments provided on your website. For many years I’ve practiced a modified form of Trigger Point Therapy, and the patterns of pink and redness induced during my very brief treatment sessions match some of the illustrations shown on your pages. Thank you!
Feel free to delete this comment, but a chunk of this article above is repeated, which makes for tricky reading until you realize you can keep scrolling to get to the rest. It would be good to fix.